If You Were 15 and Read This Article, How Should Your Future Self Respond?
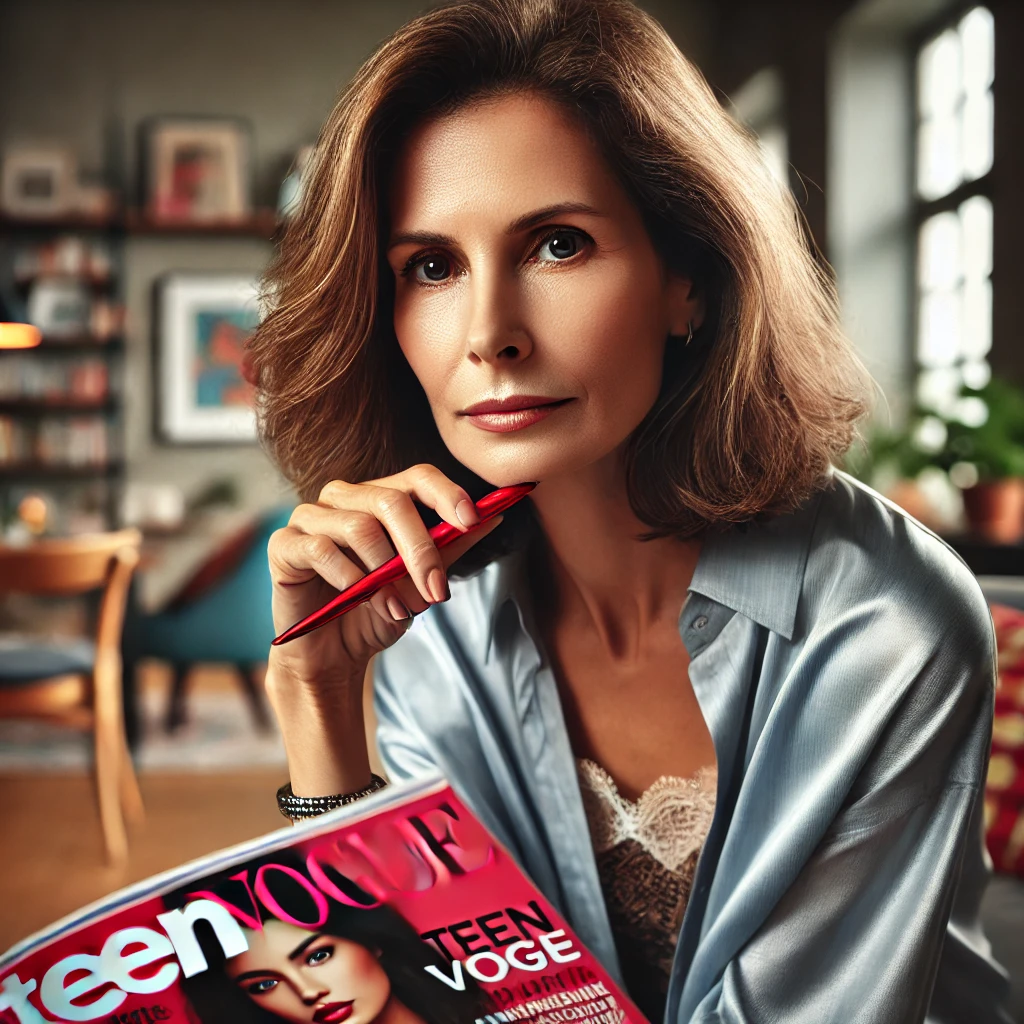
Dr. Raegan McDonald Mosley just published “Birth Control Facts and Myths: An OBGYN Answers Your Biggest Birth Control Questions” in Teen Vogue.
She is the CEO of Power to Decide and also runs Bedsider, both organizations that help you find abortion resources and ways to order birth control online.
I pray your teen daughter never reads an article like this unsupervised. But if she does, I want to help her read it like her future self.
Mosley begins:
“Birth control has revolutionized people’s ability to take charge of their health, pursue their dreams, and decide if and when to start a family.”
If you are using birth control off-label to cure an actual disease or medical condition, then yes, it may allow you to “take charge of your health” to make it better.
If an otherwise healthy teen is voluntarily taking birth control for the sole purpose of preventing birth, then she is also taking charge of her health, but to make it worse.
Taking a healthy functioning endocrine system and sabotaging it for years on end because relatives of your great grandparents were worried about overpopulation three generations ago is a curious way to take charge of your health.
“…despite its crucial role in our lives, myths and misinformation about birth control persist.”
Yes, misinformation persists. Where is it coming from?
“If you are on a pill that is working well for you, it is safe to take the birth control pill for years without a break. If you want to get pregnant or are experiencing side effects, talk to a provider about the best way for you to stop the pill. Everyone is different, and not all birth control methods work for everyone, so it may take a couple tries until you find the method that’s best for you. And, while we’re here, long-term use of the pill – does not affect your fertility once you stop taking it.”
Research indicates it takes between 1-3 months for your hormones to fully return to normal levels after long term use of hormonal contraception (HC).
But it can take longer.
Even the paper Mosley cites clearly states “…hormonal contraceptives commonly take months to clear from the body which results in temporary delay in resumption of pregnancy for months.”1
Carina Heller is not messing around. After her experiences on HC and a nearly 5-month wait for a return to normal menstruation, she scanned her brain 75 times in the name of science to find out what the heck oral contraception was doing to her body.2
“When I was 15 years old, I began using oral contraceptives to treat my acne. At 27, I decided to stop taking them, and my skin started breaking out again. I experienced light mood swings and irritability, common premenstrual symptoms I hadn’t had for the 12 years I was on oral contraceptives. Even more surprising was the fact that my menstrual cycle did not return for nearly five months.
These experiences highlighted for me the profound ways oral contraceptives can affect the body beyond their intended purposes. The medication had influenced not only my skin and cycle, but my mood and overall sense of well-being.”
I look forward to seeing her results.
A paper titled “Regulatory T Cell Proportion and Phenotype Are Altered in Women Using Oral Contraception” looks at how oral contraceptives affect T cells and the implications3:
“There is evidence that sex-steroid hormones estrogen and progesterone modulate Treg cell abundance and phenotype in women. Since natural oscillations in these hormones are modified by hormonal contraceptives, we examined whether oral contraception (OC) use impacts Treg cells and related T cell populations…
Compared to naturally cycling women, women using OC had fewer Treg cells and an altered Treg cell phenotype. Notably, Treg cells exhibiting a strongly suppressive phenotype, defined by high FOXP3, CD25, Helios, HLADR, CTLA4, and Ki67, comprised a lower proportion of total Treg cells, particularly in the early- and mid-cycle phases…
These findings imply that OC can modulate the number and phenotype of peripheral blood Treg cells and raise the possibility that Treg cells contribute to the physiological changes and altered disease susceptibility linked with OC use.” (Moldenhauer, et al., 2022)
And what do Treg cells have to do with fertility?
“In addition to autoimmune disorders, alterations in Treg cell populations are implicated in unexplained infertility and obstetric disorders. Treg cell deficiency causes pregnancy loss in animals models, and in women, aberrant Treg cell populations are linked to pregnancy pathologies including preterm labor, preeclampsia, and miscarriage.
It is well-established that prior OC use does not impair capacity to later conceive a healthy pregnancy, but a short-term delay of 2 to 6 months in the return of fertility after OC use has been reported.
Other studies suggest that OC use prior to pregnancy can elevate the risk of pregnancy complications, and there is conflicting evidence on links between OC use and miscarriage. Whether any effects of OC on maternal Treg cells could carry through into pregnancy remains to be investigated.” (Moldenhauer, et al., 2022)
A paper by Nassaralla et al. in 2011 titled “Characteristics of the Menstrual Cycle After Discontinuation of Oral Contraceptives”4 concludes:
“Statistically significant differences in several biomarkers of the women’s menstrual cycle were observed after discontinuation of OCs. These changes may help explain why there is a decrease in the chances for a couple to conceive within the first few months after discontinuation of OCs.”
Or how about this paper’s warning about future IVF difficulties5 after long-term OCP use:
“Long-term combined OCP use (5 years or more) can potentially affect optimal endometrial growth, leading to a higher cancellation rate and longer stimulation in frozen embryo transfer cycles. These findings suggest a previously unidentified adverse effect of long-term combined OCP use in women who are anticipating future fertility.”
It is well know that there is some degree of temporary infertility after using OC. But Dr. Mosley told you the pill “does not affect your fertility once you stop taking it.” Is she spreading misinformation?
Let’s continue with the article.
Regarding fertility awareness methods (FAM), she writes:
“Still, even with all the right measures in place, these methods aren’t the most effective because they need to be practiced pretty perfectly, which can be hard for most people.”
The same can be said for the pill; it can be 97% effective when used perfectly. But not all women use it perfectly. That’s why the “typical use” effectiveness rate is around 93%.
What does the research say about FAM effectiveness?
Regarding the Billing method, this 2023 study6 showed a 97% effectiveness rate. PI in the article represents how many unintended pregnancies per 100 women in 1 year (or 13 cycles). The symptothermal method was 99.5% effective.
“According to a 1981 WHO multicenter trial, 97% of women had an excellent or good understanding of the [Billing] method after 3 cycles. After a 16-cycle trial, the PI was 2.8, considering only method-related pregnancies…
A prospective cohort study involving 900 women evaluated the efficacy of the symptothermal method over a 13-cycle observation period, which can be roughly compared to the PI (12-month observation period). The unintended pregnancy rate per 100 women per year (13 cycles) was 1.61, which decreased to 0.43 with accurate use of the symptothermal method (i.e. with total abstinence during the fertile period).” (Genazzani, Fidecicchi. Arduini, Giannini, & Simoncini, 2023)
But beware these methods, they say. Because you have to actually learn how to use them. (Gasp!)
Mosley continues:
“Plus, for fertility awareness methods to be effective, your cycle needs to be regular and between 26 and 32 days long. If your cycle is shorter or longer than that more than twice during a year, fertility awareness methods won’t be effective.” (emphasis mine)
Mosley links this paragraph to a page on the Planned Parenthood website7. As you can see, part of the article talks about the Standard Days Method:
“The Standard Days Method is a variation on the calendar method. You track your menstrual cycle for several months to figure out if your cycle is always between 26 and 32 days long — you can’t use this method if it’s longer or shorter.” (Planned Parenthood) (emphasis mine)
Mosley is conflating the Standard Days Method with all fertility awareness methods.
Is this an honest mistake?
Regardless, this is a clear example of misinformation.
I would love to have seen more research studies cited other than the one. But 12 out of 18 links were to Bedsider (8) and Teen Vogue (4).
“We know that birth control has empowered people to take control of their reproductive well-being.”
No. It has given women some autonomy. At an expense. The extent of which is still to be determined.
“Birth control is health care, and it’s not controversial—it’s essential.”
It’s naive to think the people who want you on birth control care about your health.
But they sure don’t want you to have a baby.
Exogenous hormones might help manage actual diseases or medical conditions.
But pregnancy is not a disease.
And show me a birth control pill that ever made a healthy woman healthier.
- Girum, T., & Wasie, A. (2018). Return of fertility after discontinuation of contraception: a systematic review and meta-analysis. Contraception and reproductive medicine, 3, 9. https://doi.org/10.1186/s40834-018-0064-y ↩︎
- https://www.thetransmitter.org/brain-imaging/dose-scan-repeat-tracking-the-neurological-effects-of-oral-contraceptives/ ↩︎
- Lachlan M Moldenhauer, Min Jin, Jasmine J Wilson, Ella S Green, David J Sharkey, Mark D Salkeld, Thomas C Bristow, M Louise Hull, Gustaaf A Dekker, Sarah A Robertson, Regulatory T Cell Proportion and Phenotype Are Altered in Women Using Oral Contraception, Endocrinology, Volume 163, Issue 9, September 2022, bqac098, https://doi.org/10.1210/endocr/bqac098 ↩︎
- Nassaralla, C. L., Stanford, J. B., Daly, K. D., Schneider, M., Schliep, K. C., & Fehring, R. J. (2011). Characteristics of the menstrual cycle after discontinuation of oral contraceptives. Journal of women’s health (2002), 20(2), 169–177. https://doi.org/10.1089/jwh.2010.2001 ↩︎
- Talukdar, Nayana MBBS, MD; Bentov, Yaakov MD, MSc; Chang, Paul T. MD, FRCS(C); Esfandiari, Navid PhD; Nazemian, Zohreh MD, MSc; Casper, Robert F. MD, FRCS(C). Effect of Long-Term Combined Oral Contraceptive Pill Use on Endometrial Thickness. Obstetrics & Gynecology 120(2 Part 1):p 348-354, August 2012. | DOI: 10.1097/AOG.0b013e31825ec2ee ↩︎
- Genazzani, A. R., Fidecicchi, T., Arduini, D., Giannini, A., & Simoncini, T. (2023). Hormonal and natural contraceptives: a review on efficacy and risks of different methods for an informed choice. Gynecological Endocrinology, 39(1). https://doi.org/10.1080/09513590.2023.2247093 ↩︎
- https://www.plannedparenthood.org/learn/birth-control/fertility-awareness ↩︎

Hi i am kavin, its my first time to commenting anywhere, when i read this
article i thought i could also create comment due to this sensible paragraph.
Feel free to surf to my website :: click here
I was excited to discover this site. I need to to thank you
for ones time due to this wonderful read!! I definitely savored every little bit of it and i also have you saved
as a favorite to look at new information on your web
site.
Feel free to surf to my web site: click here