When the Conscience is Based on Hopes and Dreams
How do birth control pills “primarily” work?
Scour the internet and you’ll find terms like “primary mode of action” and “primary mechanism of action.”
Here is the distinction:
“Mechanism of action: Biological response derived from a drug administration, due to the interaction of the molecule with specific protein targets. It defines the functional changes on a molecular level, in contrast with ‘mode of action’, which instead refers to the changes observed after administration of a substance on a cellular level.”1 (Liggi, 2014, p. 2030)
To keep things simple, I’m going to use both terms interchangeably. Sorry, molecular biologists.
A more important distinction for this discussion is when and why the word “primary” is supposed to be used when referring to mode or mechanism of action.
The Code of Federal Regulations Title 21 includes extensive definitions, but here’s the gist:
The term “primary mode of action” is reserved for combination products.
Combined-oral-contraceptives like Yaz fit this category because they are comprised of more than one drug.
But progesterone-only-pills like Opill are not a combination product since they are comprised of a single drug. Therefore, you would expect to see simply a “mode of action” described without anything labeled as primary.
Let’s take a look at how these products are described on the web, and then we’ll look at how they’re described by the FDA label.
Yaz
From Mayoclinic.org:
“It is a birth control pill that contains two types of hormones, ethinyl estradiol and drospirenone, and when taken properly, prevents pregnancy. It works by stopping a woman’s egg from fully developing each month. The egg can no longer accept a sperm and fertilization (pregnancy) is prevented.”2
According to Mayo, it simply prevents ovulation.
From Forhers.com:
“These two hormones work together to prevent pregnancy. The process by which Yaz works is surprisingly simple: by increasing your body’s levels of drospirenone and ethinyl estradiol, Yaz can stop your ovaries from releasing eggs (a process known as ovulation)…The combination of drospirenone and ethinyl estradiol in Yaz also changes the lining of your uterus and the mucus surrounding your cervix, making it more difficult for sperm to enter into your uterus and cause pregnancy.”3
According to Forhers.com, it also changes the lining of the uterus and the cervical mucus.
From Drugwatch.com:
“Yaz prevents pregnancy in two ways. Hormones in the drug prevent your ovaries from releasing eggs. They also thicken your cervical mucus and thin your uterine lining, making it difficult for sperm to travel or for a fertilized egg to attach to your uterine wall.”4
More mention of the uterine lining.
From the National Library of Medicine:
“COCs lower the risk of becoming pregnant primarily by suppressing ovulation. Other possible mechanisms may include cervical mucus changes that inhibit sperm penetration and the endometrial changes that reduce the likelihood of implantation.”5
Mention of endometrial changes.
And here is the text from the FDA label for Yaz:
Mechanism of Action
“COCs lower the risk of becoming pregnant primarily by suppressing ovulation. Other possible mechanisms may include cervical mucus changes that inhibit sperm penetration and the endometrial changes that reduce the likelihood of implantation.”6
The official label claims that it primarily suppresses ovulation.
The problem with this claim—and most claims about ovulation rates—is that studies use indirect evidence to estimate ovulation rates.
“The end point for defining whether ovulation has occurred during use of hormonal contraception has been detection of a positive pregnancy test at the end of a menstrual cycle rather than by detection of ovum release by the Graafian follicle. This has led to confusing and inconsistent definitions of ovulatory activity as noted in a systematic review by van Heusden, Coelingh Bennink, and Fauser (2002). This situation persists to date.”7 (Harrison, Buskmiller, Chireau, Ruppersberger, Yeung, 2018, p. 454)
Criteria have been developed (Hoogland scoring system described in 1993) that include measuring follicle size and change over time via ultrasound combined with hormone level measurements that when taken together lead researchers to believe ovulation probably did or did not occur. They can’t see the actual egg on an ultrasound and they’re not sending in a camera. The method of verification is a positive pregnancy test—which begs the question: how do they confirm with certainty ovulation if there was a preclinical loss prior to detectable levels of HcG used by a pregnancy test?
They don’t.
Harrison continues:
“…all of the current proxy criteria for detection of ovulation have an unspecified false-negative rate. Moreover, none of the proxy measures has been definitely correlated with egg release. Each has been demonstrated in some studies to miss actual egg release, and each has been correlated to a pregnancy rate greater than zero in cases not classified as ovulation. This is an important point to consider when evaluating studies of ovulation rates with hormonal contraceptives, which state that no ovulation occurred during the use of a particular method of contraception.” (Harrison et al., 2018, p. 456)
So if Yaz is a combination product which merits a “primary” mode of action description, why did so few of these resources throw down with which mode was primary? Could it be that they’re unsure?
Let’s now let’s look at Opill.
Opill (Progestin-only-pill)
Here’s a description from healthcare.utah.edu:
“Well, how does it work? Well, the combination pill with estrogen works by blocking ovulation. That’s its primary mechanism of action. It also changes the cervical mucus so it’s not so likely for the sperm to get up there. That’s the progestin action. And it changes the lining, so it’s not likely to be a good place for anything to grow. Its primary mechanism of action, although this is the combination pill with estrogen, is to block ovulation.”8
Why are they describing a primary mechanism of action for a single-drug product? How are they sure? This is a conclusion based on what they hope to be the primary mechanism of action based on indirect evidence. Once again, they acknowledge endometrial effects.
From PlannedParenthood:
“Like all birth control pills, Opill works by stopping sperm from joining with an egg a few different ways. If sperm and egg don’t meet, pregnancy can’t happen. The hormones in Opill safely stop ovulation. No ovulation means there’s no egg released from the ovaries for sperm to get to. Opill’s hormones also thicken the mucus on your cervix. This thicker cervical mucus blocks sperm so it can’t swim to an egg — kind of like a sticky security guard.”9
Planned Parenthood makes no mention of endometrial effects.
This is from theconversation.com:
“Opill contains norgestrel, which is a synthetic form of the hormone progesterone. Progesterone works in several ways to prevent pregnancy. First, it thickens the mucus in the cervix, which makes it challenging for sperm to enter the uterus and fertilize an egg. Second, it thins the lining of the uterus, making it less hospitable for a fertilized egg to implant. And third, it can prevent ovulation, or release of the egg, in most people.”110
Thickening the mucus is first on the list. They do mention endometrial effects. And preventing ovulation is appropriately third since women taking POPs tend to ovulate 43% of the time11 (Milson, Korver, 2008), or 40% of the time according to a CNN article.12
From KaiserPermanente.org:
“Opill is the first over-the-counter birth control pill approved by the U.S. Food and Drug Administration. It is a progestin-only pill (.075mg norgestrel) taken daily to prevent pregnancy. Opill works by thickening the mucus in the cervix, making it less likely that the sperm can enter the uterus to fertilize an egg.”13
No mention of thickening mucus. No mention of endometrial effects.
What’s a girl to think?
Now from the Opill FDA Label:
“1. Mode of Action
Progestin-only oral contraceptives such as Opill Tablets prevent conception by suppressing ovulation in approximately half of the cycles in users, thickening the cervical mucus to inhibit sperm penetration, lowering the midcycle LH and FSH peaks, slowing the movement of the ovum through the fallopian tubes, and altering the endometrium.”14
Now we’re getting somewhere. They’ve mentioned five different things that are happening. These are all the result of manipulating the hypothalamic-pituitary-gonadal (HPG) axis, and it’s time to focus on a very relevant term:
Since ovulation happens a lot on the mini-pill, something else must be responsible for it’s effectiveness. They’ll tell you that it’s that thick cervial mucus that’s doing the heavy lifting.
I’m not so sure.
Studies have proven it gets thick. But they’ve done a poor job of proving with any direct evidence that thick equals ineffective.
Could it be that embryo-endometrial desynchronization cause by slowed tubal motility and impaired endometrial decidualization cause by prolonged use of hormonal contraception (HC) could be the reason women aren’t having babies despite ovulating 40% of the time?
All this to say, the manipulation of the HPG axis by HC has many effects on the body. And it’s more than just inhibiting ovulation, thickening mucus, and altering the endometrium.
I will show you studies that suggest that using HC causes changes during the proliferative phase (pre-fertilization) that may be causing post-fertilization effects
Heres’ what happens in knock-out mice, and perhaps in humans:
“During the proliferative phase, estrogen (through ERα) causes the progesterone receptor (PR) in endometrial cells to induce progesterone responsiveness during the luteal phase…These study data can be extrapolated to humans, demonstrating the importance of progesterone receptors and their different functions in fertility.”15 (Gunther et al., 2023, p. 3)
In other words, how the endometrium responds post-fertilization depends on what is happening before fertilization. This is just one example of how pre-fertilization processes affect post-fertilization outcomes.
Here’s another:
“…in women with sporadic or chronic anovulation, there is reduced progesterone throughout the menstrual cycle (154) suggesting there is potential for altered luteal function…The formation of a functional corpus luteum relies on the appropriate proliferation and differentiation of both granulosa and theca cells. Any disruption in the crosstalk between granulosa and theca cell or differentiation of these cells types alters lineages and gene expression profiles that could negatively impact luteinization and progesterone production.” (Abedel-Majed, Romereim, Davis, Cupp, 2019, p. 11)
If you do end up conceiving while on the pill, altered luteal function is bad for babies. A common term in the artificial reproductive technology (ART) community is Luteal Phase Defect (where the body fails to produce enough progesterone after ovulation), and it’s likely one of the reasons IFV fails 70% (or more based on age) of the time.
Taking a progestin pill every day is not pumping you full of good hormones. It’s keeping your natural progesterone extremely low. The pill causes reduced progesterone throughout the menstrual cycle.
Reading Between the Lines
Let’s look at a study on sugammadex. What does sugammadex have to do with HC? Nothing! It’s a drug used as a reversal agent for muscle relaxants. But let’s read between the lines of the study and glean what we can as it relates to hormone levels on HC. Part of the study involved measuring the baseline levels of progesterone of women using hormonal contraception.
Out of the 122 participants included in the study, 60 were part of the “case group” and were using hormonal contraception.
“For the purpose of analysis, oestrogen and progesterone samples that were below the level of detection for the assay were recorded as 5 pmol.l−1 and 0.2 nmol.l−1, respectively. This occurred once in oestrogen sampling (in the case group) and 84 times in progesterone sampling: 52 times in the case group; 23 times in control A; and 8 times in control B (emphasis mine).”16 (Devoy, Hunter, Smith, 2022.)
52 out of 60 women using HC had baseline levels of progesterone less than .2 nmol/L—undetectable by the assay!
What are the progesterone levels of a healthy woman during normal menstruation? According to forthwithlife.co.uk:
“Progesterone levels are low during the first phase of the menstrual cycle, called the ‘follicular phase’, ranging between 0-0.6nmol/L. During ovulation, levels rise to 0.2-13.2nmol/L. They rise again after ovulation, known as the ‘luteal phase’, to between 13.1-46.3nmol/L.”17
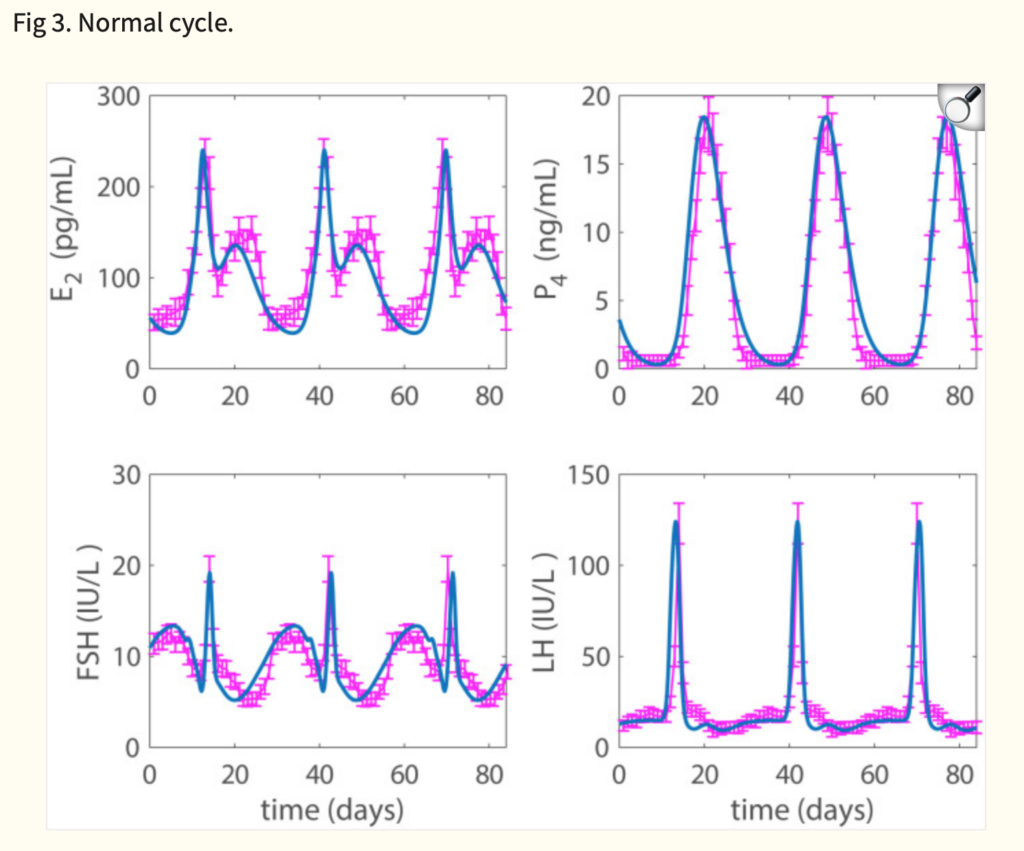
(See Fig.3 of this other source [Wright, Fayad, Selgrade, Olufsen, 2020] for normal progesterone (P4) levels [not on HC].18 18 ng/mL [peak] is equal to about 57 nmol/L.)
The Devoy et al. study does not include at what point in a woman’s cycle the three blood samples were taken, but based on the nature of continuously administered HC, it’s a reasonable assumption that the baseline measurement persists unless there is a placebo-based withdrawal bleed.
Why were their baseline levels of progesterone so low? Because that’s what HC is designed to do.
“Participants in the case group demonstrated low baseline hormone concentrations, likely due to physiological suppression by exogenous hormones…We speculate that the very low baseline progesterone concentrations in women on contraception make it less likely for an external drug such as sugammadex to cause meaningful decreases.” (Devoy et al., 2022, p. 183)
Normal cycle: progesterone rises to between 13-46 nmol/L
On continuous HC: progesterone remains at or below 0.2 nmol/L
Despite this being a study on summadex, what it tells HC researchers is that HC keeps progesterone REALLY low.
Like, undetectable low.
This is important because some authors like C. Ryan Fields quote an article by Sullivan in 2006 that theorizes (without any data) that the corpus luteum can somehow restore sufficient and syncrhronized progesterone levels in the event of ovulation following a prolonged HC-induced low progesterone state.
“‘If [breakthrough] ovulation takes place, a completely different hormonal milieu comes into existence [because] ovulation leaves behind the corpus luteum, a rich source of estrogen and progesterone. After the six days required for the embryo to travel down the uterine tube into the uterus, these hormones [would] have transformed the endometrium, [making it] receptive for implantation.’[31] In short, Sullivan argues that we have good reason to think that the ‘hostile endometrium’ pointed to by the pill’s opponents is, by the time of implantation, actually transformed into a sufficiently ‘hospitable’ one.”18 (Fields, 2020, p. 25)
But there is some data.
The Elusive Data
Some of the hardest data to get is of hormone levels in the event of ovulation while on HC. I’ve already mentioned how ovulation rates are usually measured indirectly. But some studies may warrant additional credibility, such as studies that are specifically designed with that end in mind.
A study by Birth, Olatunbosun, and Pierson in 2006 captured two instances of ovulation while on HC and reported the progesterone levels. Both women were on combined oral contraceptives. One woman was on a regimen of 30 mcg EE (ethinyl estradiol) /150 mcg LNG (levonorgestrel). The other was on a regimen of 35 mcg EE/250 mcg NGM (norgestimate).
In addition to measuring hormones via blood sampling and follicles via transvaginal ultrasonography, the corpus luteum was also imaged.
Normally, when a woman ovulates (not on HC), the progesterone level 6-8 days after ovulation is increased as high as 18 ng/mL (57 nmol/L).
In these two instances of ovulation while on the pill, the first woman’s progesterone measured 0.79 ng/mL six days after ovulation. The second woman measured 3.5 ng/mL 8 days after ovulation.19 (Birtch, Olatunbosun, Pierson, 2006)
These progesterone levels of women who ovulated while on hormonal contraceptives is around 6-18 times less than normal.
This is exactly the time that the embryos would be implanting in the uterus if conception occurred. Studies suggest progesterone needs to be generally above 10 ng/mL at this time for a successful pregnancy outcome.
In other words, here are two documented cases where women probably ovulated while on HC, and during the crucial implantation period (in the event of conception), hormone levels were far from restored by the corpus luteum to anything close to above 10 ng/mL.
The Endometrium is Selective
Some studies have described how the endometrium “selects” which embryos to accept based on maternal-fetal cross-talk via biological mechanisms throughout the pregnancy process. When the endometrium gets sick/confused due to the effects of HC, it may not be in its right mind, so to speak.
That means that not only may the endometrium fail to gestate good embryos, but it may also attempt to gestate embryos that would normally be destined for failure.
“Recent experimental evidence has led to the concept that the decidualized endometrium acts as biosensor of embryo quality, which if disrupted, may lead to implantation of embryos destined to miscarry.”20 (Larsen, Christiansen, Kolte, Macklon, 2013)
Embryos that would normally be lost early without the knowledge of the mother are potentially being lost later in pregnancy, with all the associated heartache and pain.
If all this is the case, Protestants are going to have a few new pills to swallow.
- Liggi, S., Drakakis, G., Koutsoukas, A., Cortes-Ciriano, I., Martínez-Alonso, P., Malliavin, T. E., Velazquez-Campoy, A., Brewerton, S. C., Bodkin, M. J., Evans, D. A., Glen, R. C., Carrodeguas, J. A., & Bender, A. (2014). Extending in silico mechanism-of-action analysis by annotating targets with pathways: application to cellular cytotoxicity readouts. Future medicinal chemistry, 6(18), 2029–2056. https://doi.org/10.4155/fmc.14.137 ↩︎
- Mayo Clinic. (Accessed 2024, October 15). Drospirenone and ethinyl estradiol (oral route).Mayoclinic.org. https://www.mayoclinic.org/drugs-supplements/drospirenone-and-ethinyl-estradiol-oral-route/description/drg-20061917# ↩︎
- Hers. (2021, September 2). Drospirenone & Ethinyl Estradiol (Yaz) 101: How it Works, Side Effects and Interactions.Forhers.com. https://www.forhers.com/blog/drospirenone-ethinyl-estradiol-yaz-101-how-it-works-side-effects-and-interactions ↩︎
- Drugwatch. (2023, September 5). Yaz. Drugwatch.com. https://www.drugwatch.com/yaz/ ↩︎
- National Library of Medicine. (2012, March 15). LABEL: YAZ- drospirenone and ethinyl estradiol kit. dailymed.nlm.nih.gov. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=077bf6ff-afb8-4cb7-9faa-fbb6fd9f037f ↩︎
- FDA. (2012, April). HIGHLIGHTS OF PRESCRIBING INFORMATION. access data.fda.gov. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021676s012lbl.pdf ↩︎
- Harrison, D., Buskmiller, C., Chireau, M., Ruppersberger, L. A., & Yeung, P. P., Jr (2018). Systematic Review of Ovarian Activity and Potential for Embryo Formation and Loss during the Use of Hormonal Contraception. The Linacre quarterly, 85(4), 453–469. https://doi.org/10.1177/0024363918815611 ↩︎
- University of Utah Health. (2023, Jul 28). What you need to know about Opill, the first FDA-approved over-the-counter birth control pill. healthcare.utah.edu. https://healthcare.utah.edu/the-scope/health-library/all/2023/07/what-you-need-know-about-opill-first-fda-approved-over-counter ↩︎
- Planned Parenthood. (2024, March 8). The first over-the-counter birth control pill is here: what you need to know. plannedparenthood.org. https://www.plannedparenthood.org/blog/the-first-over-the-counter-birth-control-pill-is-here-what-you-need-to-know ↩︎
- The Conversation. (2023, July 19). How does the new over-the-counter birth control pill, Opill, work to prevent pregnancy? 5 questions answered. theconversation.com. https://theconversation.com/how-does-the-new-over-the-counter-birth-control-pill-opill-work-to-prevent-pregnancy-5-questions-answered-209801 ↩︎
- Milsom, I., & Korver, T. (2008). Ovulation incidence with oral contraceptives: a literature review. The journal of family planning and reproductive health care, 34(4), 237–246. https://doi.org/10.1783/147118908786000451 ↩︎
- CNN. (2023 July 21). The FDA approved the US’ first over-the-counter birth control pill. What happens next? cnn.com. https://www.cnn.com/2023/07/21/health/opill-birth-control-wellness/index.html ↩︎
- Kaiser Permanente. (2024, April 9). Opill: First Nonprescription Birth Control Pill. mydoctor.kaiserpermanente.org. https://mydoctor.kaiserpermanente.org/mas/news/opill-first-nonprescription-birth-control-pill-2445060 ↩︎
- FDA. (2017, August). Opill® Tablets. accessdata.fda.gov. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/017031s035s036lbl.pdf ↩︎
- Günther, V., Allahqoli, L., Deenadayal-Mettler, A., Maass, N., Mettler, L., Gitas, G., Andresen, K., Schubert, M., Ackermann, J., von Otte, S., & Alkatout, I. (2023). Molecular Determinants of Uterine Receptivity: Comparison of Successful Implantation, Recurrent Miscarriage, and Recurrent Implantation Failure. International journal of molecular sciences, 24(24), 17616. https://doi.org/10.3390/ijms242417616 ↩︎
- Devoy, T., Hunter, M., & Smith, N. A. (2023). A prospective observational study of the effects of sugammadex on peri-operative oestrogen and progesterone levels in women who take hormonal contraception. Anaesthesia, 78(2), 180–187. https://doi.org/10.1111/anae.15902 ↩︎
- Forth. (2020, November 3). Progesterone Levels In Women. forthwithlife.co.uk. https://www.forthwithlife.co.uk/blog/progesterone-levels-in-women/# ↩︎
- Fields, Ryan C. (2020). The Christian and Oral Contraceptives: An Investigation into Moral Permissibility. Dignitas, Vol. 27, No. 1-4 (Spring–Winter 2020) pp. 20-27. https://www.cbhd.org/dignitas-articles/the-christian-and-oral-contraceptives-an-investigation-into-moral-permissibility ↩︎
- Birtch, R. L., Olatunbosun, O. A., & Pierson, R. A. (2006). Ovarian follicular dynamics during conventional vs. continuous oral contraceptive use. Contraception, 73(3), 235–243. https://doi.org/10.1016/j.contraception.2005.09.009 ↩︎
- Larsen, E. C., Christiansen, O. B., Kolte, A. M., & Macklon, N. (2013). New insights into mechanisms behind miscarriage. BMC medicine, 11, 154. https://doi.org/10.1186/1741-7015-11-154 ↩︎

